Written by Kimberley Gittens, RD on behalf of Rachel McBryan, RD
You’ve been told to follow the low-FODMAP diet. But now what?
There are many reasons why you may have been told to follow a low-FODMAP diet. Understanding the diet and its underlying principles can help you more effectively follow the diet, support a healthy relationship with food, and manage your GI symptoms.
What is the Low-FODMAP Diet?
As the name suggests, the low-FODMAP diet eliminates foods with high FODMAP content from your diet. FODMAPs is an acronym for Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols.
Oligo-, di- and monosaccharides are different types of sugar, ranging from the simple sugar building blocks up to complex carbohydrates. Polyols are another type of carbohydrate that contains a hydroxyl group. While some of these sugars and carbohydrates are easily broken down and absorbed in your small intestine, other sugars and carbohydrates are more resistant to digestive enzymes, and will move into your large intestine (colon), where they are fermented by your gut bacteria.
The bacterial fermentation of these carbohydrates is responsible for many symptoms and discomfort some people experience after eating these foods. Symptoms can include,
-
- Stomach bloating
- Cramping
- Gas and flatulence
- Diarrhea
- Constipation
You can find FODMAPs in a wide variety of food, from fruits and vegetables to dairy and artificial sweeteners. You can find sources of each type of FODMAP below.
Oligosaccharides
Oligosaccharides are primarily found in wheat, rye, legumes and some fruits and vegetables. Unfortunately, this includes garlic and onions.
Disaccharides
Lactose is the main disaccharide fermented in our large intestine. You can be find it in many dairy products, including soft cheeses, yogurt and milk, as well as in some bread, cereals and candies.
Monosaccharides
Of the 3 monosaccharides, fructose is the primary culprit for resisting breakdown and alternative is fermented by gut bacteria. Fructose is found in the well-known high-fructose corn syrup, as well as in fruits (such as mangoes and figs) and natural sweeteners (such as honey and agave nectar).
Polyols
Not only can polyols be found in fruits and vegetables (such as blackberries), but they are also found in some popular low-calories sweeteners.
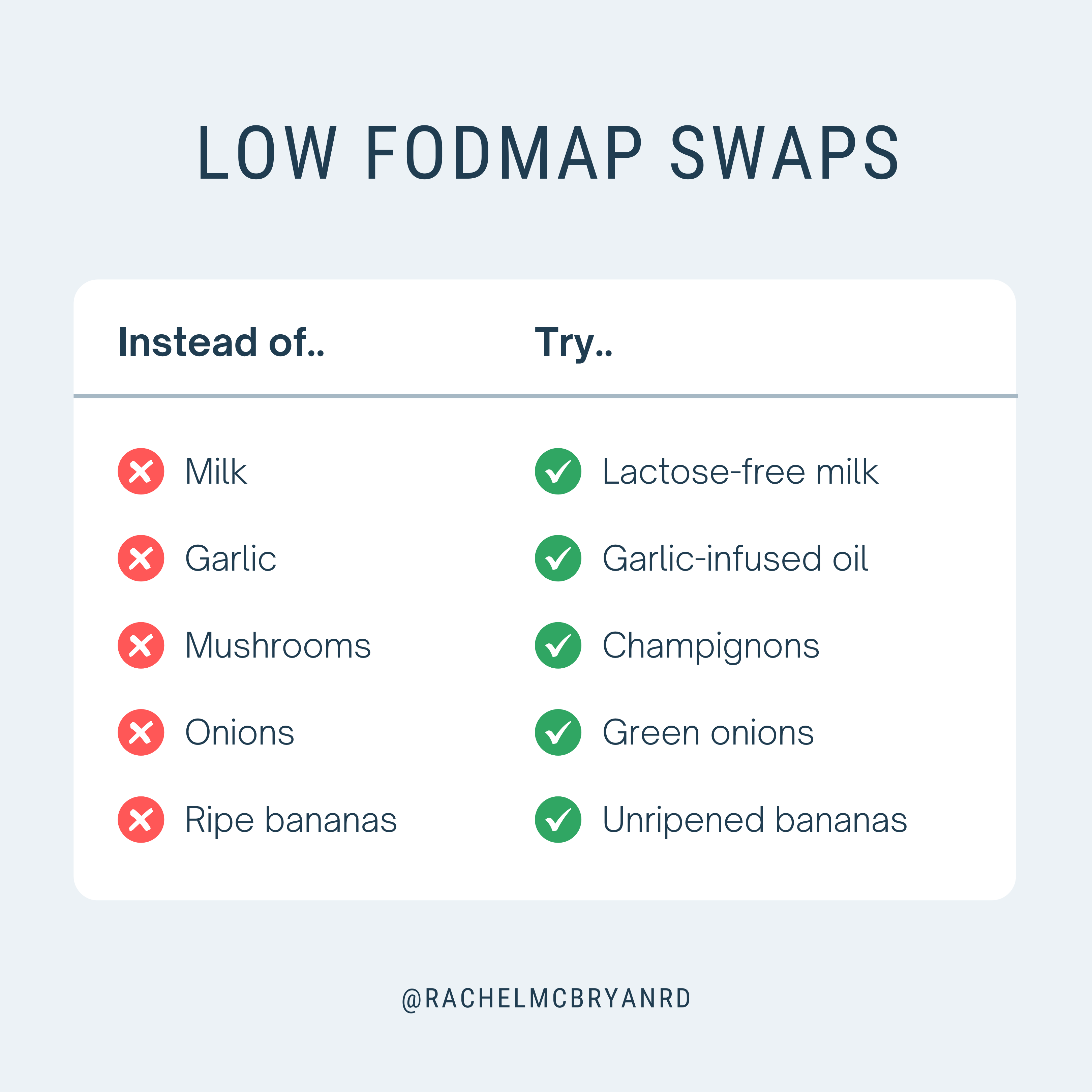
Check out this blog post for more foods and ingredients that contain high amounts of FODMAPs. Despite the long list of high-FOMDAP foods for you to avoid, there are many low-FODMAP alternatives to include in your diet.
When Is the Low-FODMAP Diet Required?
The low-FODMAP diet is commonly used by people with irritable bowel syndrome (IBS) but it can also be used for other GI conditions such as,
-
- Inflammatory bowel disease (Crohn’s disease and Ulcerative Colitis)
- Small intestine bacterial overgrowth (SIBO)
High-FODMAP foods can aggravate and trigger some GI symptoms. Studies have shown the low-FODMAP diet can help alleviate GI symptoms and reduce the frequency of flare-ups, particularly for people with IBS. Following a low-FODMAP diet with the assistance of a Registered Dietitian can help you identify your personal trigger foods and improve your management of GI conditions.
What You Need Know about the Low-FODMAP Diet
There are a few details that you should know about the low-FODMAP diet. The most important being it is not a long-term diet. It is a temporary, multi-stage diet that includes eliminating all high-FODMAP foods from your diet for 4 to 8 weeks to stop symptoms before slowly re-introducing foods.
The low-FODMAP diet is a restrictive diet and should be followed with the supervision and guidance of a healthcare procession such as a Registered Dietitian (RD) to ensure you continue to meet your nutritional needs while on the low-FODMAP diet.
What to Expect From the Low-FODMAP Diet
In the first stage of the diet, we eliminate all high-FODMAP foods from your diet, including mushrooms, honey, and broccoli. All of it. We do this to remove all the potential triggers and aggravators of a condition (whether IBS, Crohn’s, Ulcerative Colitis or SIBO) and allow the inflammation to subside.
Once we remove all the triggers are removed from your diet, inflammation will subsides and allows your GI tract begins to heal. We can then start to slowly reintroduce foods into our diet. This doesn’t mean we just add back in everything in bulk we took out. We need to slowly re-introduce high FODMAP foods, one at a time, into your diet while also keeping a food journal to track nutrient intake and associated symptoms.
Re-integrating high FODMAP foods into your diet isn’t a linear process. As different high FODMAP foods are re-introduced to our diet, they may aggravate GI conditions or trigger flare-ups of symptoms. The re-introduction of foods is a unique process for each person and occurs at different paces.
Building Low-FODMAP Meals You Enjoy
Although the low-FODMAP diet eliminates many ingredients from your plate, you can still enjoy the food you eat. Low-FODMAP swaps are one of the simple but effective strategies you can use to minimize your high-FODMAP intake and alleviate unpleasant symptoms. There are many low FODMAP alternatives available including fruits, vegetables, seasonings, sweeteners, dairy products, bread and candies to keep your diet delicious and cravings satisfied.
Visit my article to learn more about building low-FODMAP breakfasts you’ll enjoy! You can also find inspiration for low-FODMAP snacks for your busy days!
Get Help Identifying Your IBS-Triggers
Identifying your IBS triggers allows you to eliminate them from your diet, and prevent flares up and post-meal discomfort. Book a FREE discovery call today to learn more about working with a Registered Dietitian to manage your IBS!
References
Carabotti, M., Scirocco, A., Maselli, M. A., & Severi, C. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Annals of Gastroenterology : Quarterly Publication of the Hellenic Society of Gastroenterology, 28(2), 203. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/
High and Low FODMAP Foods. (n.d.). Monash University. Retrieved January 4, 2023, from https://www.monashfodmap.com/about-fodmap-and-ibs/high-and-low-fodmap-foods/
Low FODMAP Diet for Irritable Bowel Syndrome | IBS Treatment. (n.d.). Gastroenterology Consultants of San Antonio. Retrieved April 27, 2022, from https://www.gastroconsa.com/patient-education/irritable-bowel-syndrome/low-fodmap-diet/
Kimberley is a Registered Dietitian, licensed in Ontario. She helps clients across Ontario control their blood sugars and reduce their risk of chronic conditions.

